Thousands of cancer patients in the Commonwealth are paying as much as five grand a month for new cancer treatments taken orally. “Patients are having to make really difficult decisions. Do they get their prescription filled or do they put food on the table? Do they pay their monthly mortgage expenses,” said Danielle Bubnis who works at the Leukemia & Lymphoma Society.
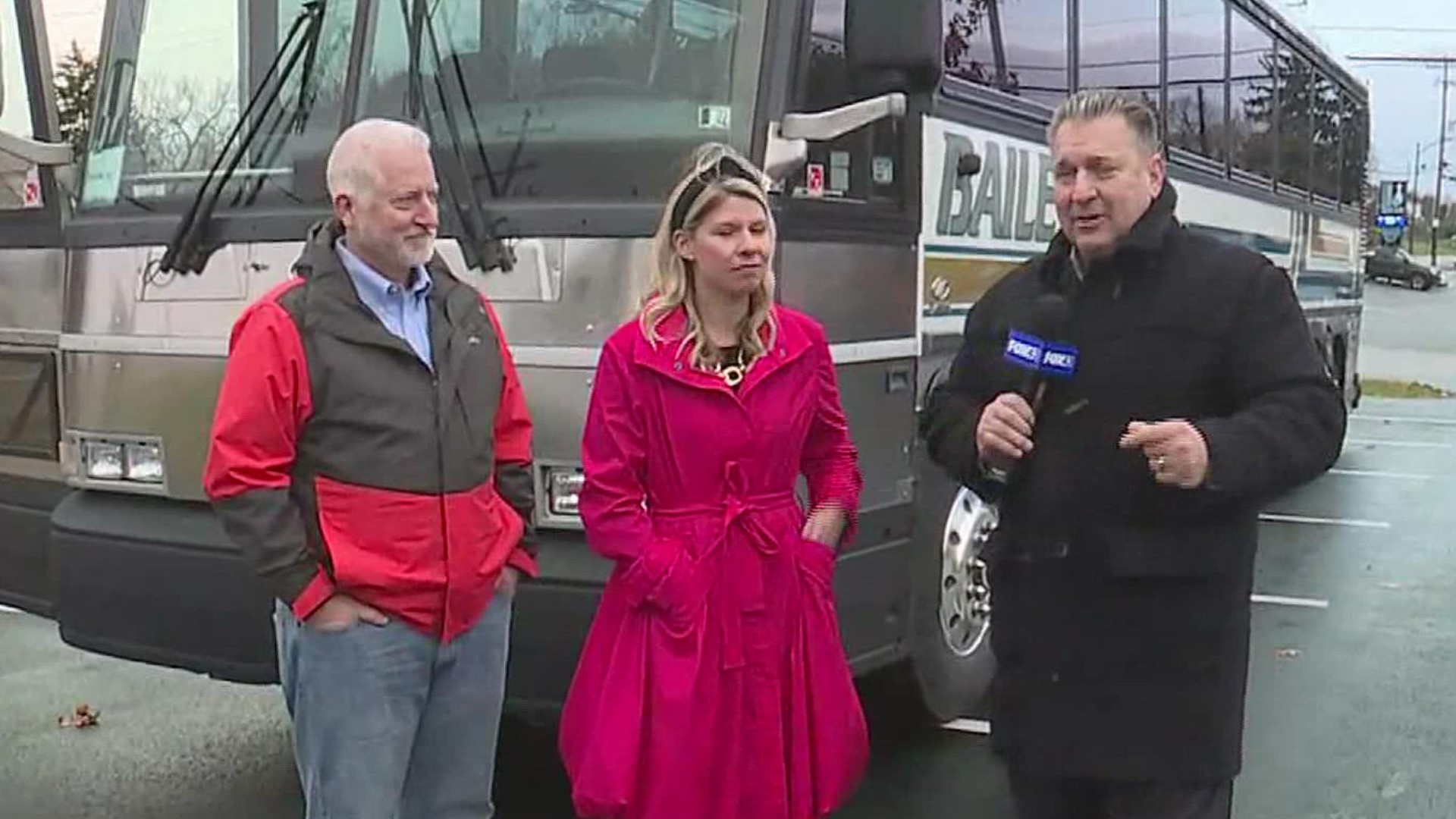
Those choices are tough, but currently they're necessary because most insurance companies won't cover the new treatments. They only cover more traditional forms of treatment like chemotherapy administered with a needle. "This discriminatory business practice of treating oral medicine differently than IV medicine, we want to level the playing field and make it more affordable and not cost prohibitive," said Republican Representative Matthew Baker who has sponsored legislation that would stop insurance companies from denying the oral medicines.
The bill has already passed in the House and is now moving through the Senate. Baker said the bill has bipartisan support and the only opposition is coming from the insurance companies. "Three states just legalized it, that brings it up to thirty seven states now. I sure hope Pennsylvania isn't the last state to do this," said Baker.
Danielle Bubnis works with cancer patients every day at the Leukemia & Lymphoma Society and said a patients story she heard recently shows just how tough the financial burden can be. "He was having a conversation with his sixteen year old daughter and he said we're going to have to make some really difficult family decisions and she asked what that meant to the family and he said you'll either be fatherless or homeless," said Bubnis.