LANCASTER COUNTY, Pa. — An emergency room nurse said she has nightmares every night. A critical care nurse working in the ICU said walking into the hospital feels like walking into battle. A doctor of internal medicine said most of his staff have some sort of PTSD.
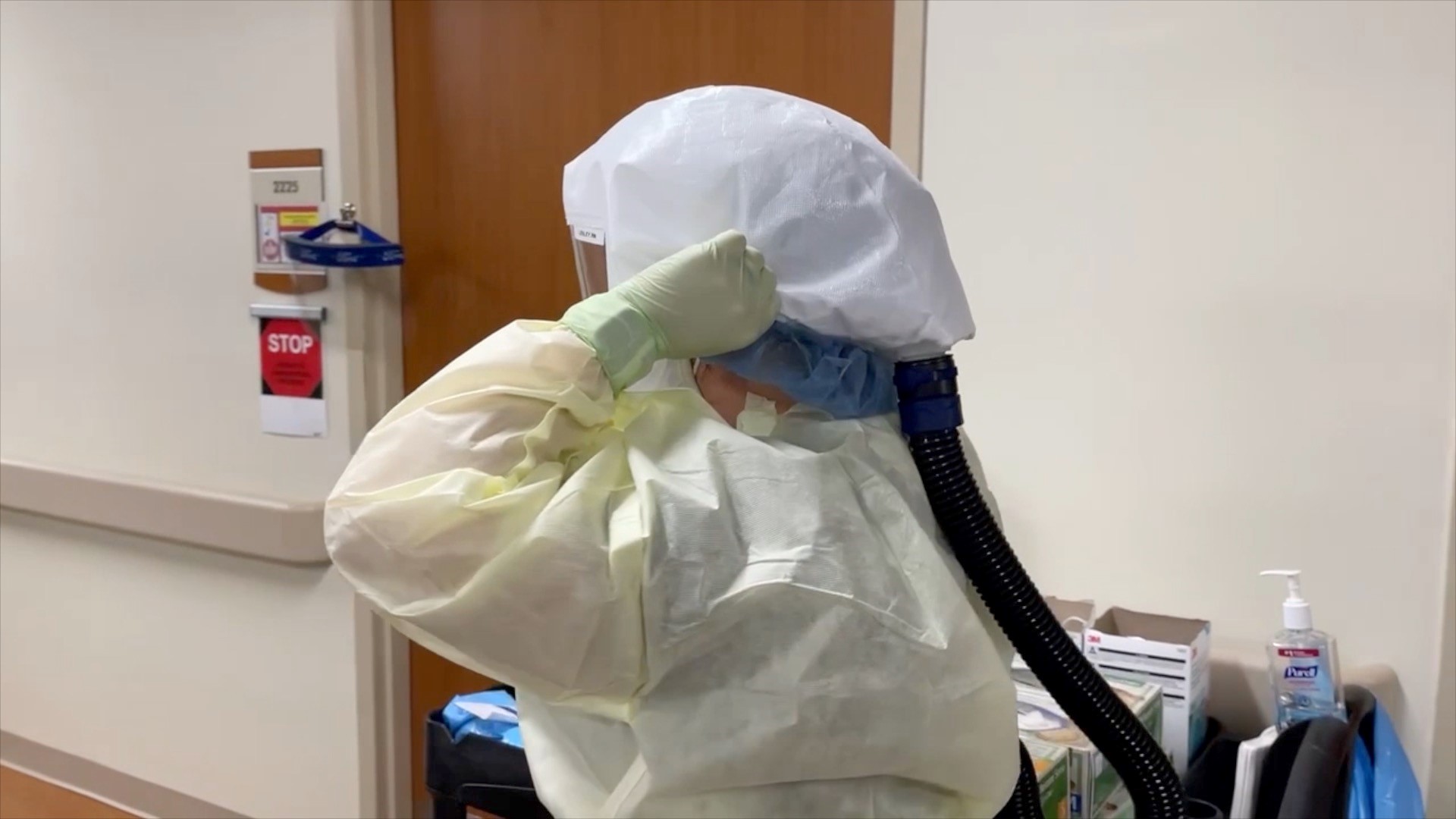
Hospitals are emerging from another wave of COVID-19. Omicron cases are fading, but staffing shortages continue to strain health care systems. FOX43 spent weeks talking with doctors and nurses about how the two-year pandemic has impacted them.
Here are some of their stories.
Erin Shock has been a nurse for 21 years. She is currently an ER nurse at UPMC Hanover, healing the very community where she grew up and continues to live today. She said her hospital has a hometown feel that is hard to come by within the health care industry.
Erin Shock: A lot of people ask me, ‘Why do you stay Erin?’ And I stay because this is my family.
Rachel Yonkunas: You can’t beat that.
Erin Shock: No, you can’t beat that. Hanover’s my home. It’s my home.
The two-year pandemic has forced nurses like Shock to make heartbreaking decisions. Hospital beds filled up with COVID patients during the Delta and Omicron waves in the winters of 2020 and 2021. At the time, health systems came close to running out of beds.
“We would have to decide who would get beds first or who was going to get which hallway bed first,” Shock said. “I’ve held people’s hands that have died in these rooms that I’ve known. I get a text later that tell me I’m so glad you were there Erin. It helps me to know you were there. That’s why I stay. Because they couldn’t be there.”
In December 2021, Pennsylvania reported more than 7,000 new daily cases of COVID-19—among the highest in the U.S. For months, hospital leaders have become increasingly concerned about another problem.
Thousands of healthcare workers are leaving the bedside. Nurses are quitting in droves at a time when baby boomers are retiring, leading to severe shortages at hospitals and nursing school programs.
More than 80,000 qualified nursing students nationwide were turned away because there were not enough faculty to teach them. The staffing crisis is pushing nurses that are still left to a breaking point.
“So many of our nurses have worked tons of overtime. Anywhere from 50, 60, 70 to 72 hours a week to fill in holes,” Shock added.
Health care facilities cannot hire staff fast enough. FOX43 Reveals that turnover rates for nurses have spiked since 2019. According to a workforce survey by the Hospital and Healthsystem Association of Pennsylvania (HAP), their member hospitals reported an average 27 percent vacancy rate for staff registered nurses (RN) providing direct patient care and a 45.5 percent vacancy rate for nursing support professionals (CNA, PCA, NA).
If these workforce shortage trends hold, a 2021 study on the U.S. healthcare labor market projects Pennsylvania will be short nearly 300,000 healthcare workers by 2026, including more than 20,000 nurses.
For nurses in the ICU, waves of new infections and deaths have left them exhausted. Statewide, less than 30% of ICU beds are available. Erin Hammond, a nurse of 18 years, is struggling to see the difference she is making in her community.
“More patients than not do not make it home once they come down here,” said Hammond, who works in critical care at WellSpan Chambersburg Hospital. “I love caring for people. I love being part of this community and knowing that I’m making a difference in this community, but it gets really hard. We all got into this job because it was our passion to help people and see people get better. Most of the time it’s a losing battle.”
Hospital staff is stretched thin even as Omicron begins to fade. One medical study found that if you are in the hospital, your chances of dying go up seven percent for every additional patient your nurse cares for. A drop in the number of new coronavirus cases, though, means hope is on the horizon.
“Unfortunately, we don’t know where this will go, but we are taking the opportunity to take a breath and kind of regroup,” said Dr. Joseph MacDonald, Co-Medical Director of the Hospitalist Program for UMPC’s Central Pennsylvania Region.
Rachel Yonkunas: Have there been any rewarding moments?
Dr. MacDonald: Absolutely. That comradery that we’ve developed, that teamwork that we’ve developed has been incredibly rewarding. They have given blood, sweat and tears throughout this process. I just think it’s really important that we continue to thank those healthcare providers.
Healthcare workers said they have developed stronger bonds with their teams during the pandemic. These relationships have been holding them together, giving them the strength to return to work each day despite the challenges.
“I am so proud to save lives besides my coworkers. They are top notch and I just would shout it from the rooftops if I could,” Shock said.
And our health care system is depending on people like them.